It’s Cervical Cancer Awareness Month. But for AO’s gynecologic oncology team, being vigilant about pelvic health is a daily endeavor.
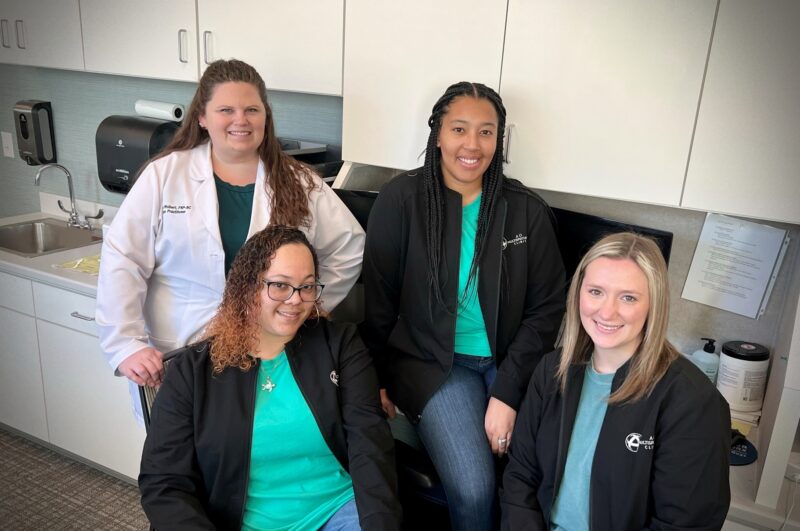
AO’s Gynecologic Oncology Care Team – from back left, clockwise: Nicole Wolbert, FNP-C; Alayna Whitten; Courtney Miller; Buffy Butler.
Nurse Practitioner Nicole Wolbert, FNP-C, leads Augusta Oncology’s gynecologic oncology team, which includes medical assistants Alayna Whitten, Buffy Butter, and Courtney Miller. As women who are caring for female patients with gynecologic cancers, the team agrees: it’s so important to stay mindful of your body’s health.
“I definitely make sure to get my annual Pap smear; don’t mess around with that,” said Alayna Whitten.
AO’s Gynecologic Oncology department treats cancers that affect the female reproductive system, including vaginal, uterine, ovarian, vulvar, and cervical cancers.
The gynecologic oncology team supports AO’s four gynecological oncologists, or “gyn oncs.” Gyn oncs Dr. Sharad Ghamande, Dr. Bunja Rungruang, Dr. Robert Higgins, and Dr. Marian Symmes Johnson hold clinic at Augusta Oncology’s downtown location.
An STI that Can Cause Cancer
Human Papillomavirus (HPV) is the most common sexually transmitted infection (STI). It’s estimated that nearly everyone who is sexually active has been exposed to a strain of the virus at some point.
There are many different types of HPV, including several strains that can lead to reproductive cancers like cervical cancer. These cancers can take years to develop, long after someone has contracted HPV. “It can lie dormant, and then come up,” said Nicole. “It’s a complicated condition.”
But HPV-related cancers are significantly more treatable when they found and treated early.
Once a Year, In the Clear
The gyn-onc team agrees: you must prioritize your annual gyn appointment.
Are you busy? Of course. Are there are other ways you’d probably rather be spending your time? Without a doubt. But the hour or so you have to sacrifice once a year to help ensure a healthy reproductive system is more than worth it.
And don’t let the fear of the unknown hold you back. “You’d be amazed at how many people just ignore little lumps and bumps,” said Nicole. “Or they might brush it off, like, ‘maybe it’s just a razor bump,'” said Alayna. If you do have an area that you’re concerned about, the earlier you get seen, the better. Waiting can exacerbate the issue and make the problem worse.
Be Your Own Advocate
While it’s important to receive regular medical care from a provider you trust, it’s equally important to trust your instincts.
The team shared an example of a female patient (being treated at a different practice) who discovered a lesion on her vulva area. The patient’s medical provider told her that they would continue to keep an eye on the lesion. But that’s not good enough, said Nicole. “Tell them to take it off and biopsy it.” Ultimately, the patient’s lesion was removed and was in fact a cause for concern.
Don’t minimize any pains or ailments that you experience. It’s important to “know what’s normal for you,” said Buffy Butler. “Know your body.”
Take a Good Look in the Mirror
The most effective way to know what’s normal for your body is to make sure you’re familiar with it. Yes, that means you need to get up close and personal “down there.”
“Just like performing self-breast exams,” explained Courtney Miller, it’s crucial to carefully check out the external parts of your body’s reproductive system. “Just check things out down there every now and then, and make sure everything is okay.” Once a month, grab a hand mirror – you can even use the reversible camera on your cell phone. Find some good lighting, and spend a few minutes examining your pelvic region carefully. Some women even get their partner to assist to make it easier.
Remember that, like your fingerprints, your body is unique. Your parts aren’t going to look the same as everyone else’s. What’s typical for someone else might not be typical for you. However, “if you know what it looks like,” said Nicole, “if something does change, you’ll be the first to know.”
A Vaccine that Could Prevent Cervical Cancer
While cancer isn’t curable, there is now a vaccine that could potentially make some types of cancer preventable. The vaccine can prevent many cases of cervical cancer, but it does need to be administered before the patient is potentially exposed to HPV. This is why the Center for Disease Control recommends that girls and boys aged 11 to 12 should be given the HPV vaccine.
It’s important to note, however, that adults as old as 45 who have already had HPV can still benefit from getting the vaccine, as it could protect you from additional virus strains.
Learn more about vaccines for HPV here.
In Summary: Cervical Cancer Awareness
Cervical cancer awareness goes beyond completing your annual gyn exam – though that’s very important, too. You must check your modesty at the door and get familiar with your body: examine it regularly. Advocate for your own health, and speak up about any concerns, no matter how trivial they may seem. Look into your options with HPV vaccination.
Above all, remember to stay observant and consistent with monitoring your health — not just during Cervical Cancer Awareness month, but every month!






